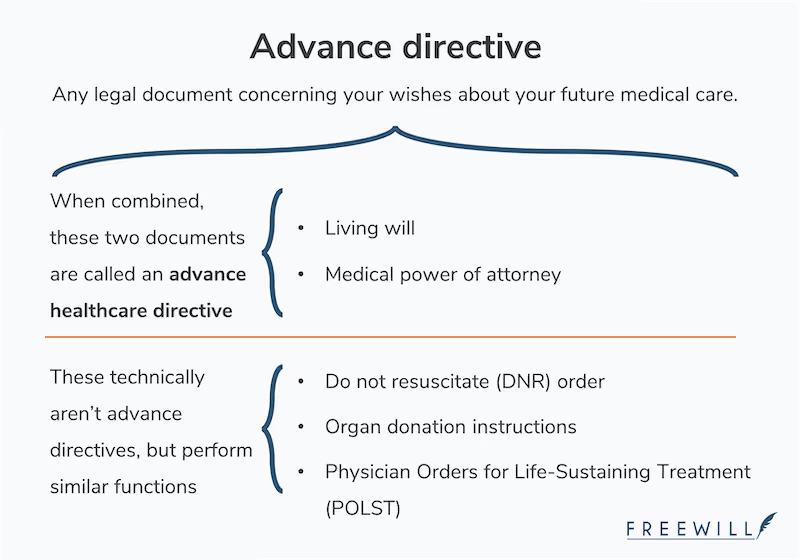
An advance directive is any legal document that lets you outline your healthcare preferences in case you’re ever unable to communicate them yourself. Your healthcare agent, doctors, and first responders will refer to your advance directives if you’re incapacitated. This helps them understand your treatment preferences and ensure you’re treated according to your wishes.
Advance directives are flexible — their scope can be broad or narrow, depending on your preferences. There are several types of advance directive documents, and there’s often overlap in what topics they cover and when they go into effect. Below, we outline some common types and the purpose each serves when it comes to your healthcare.
1. Living will
A living will is a document that lets you outline your end-of-life care preferences. You can state whether you want to receive certain medical treatments, procedures, medication, blood transfusions, and more. If you’re ever incapacitated (for example, in a coma) and can’t communicate your wishes, your doctors will consult the instructions in your living will and try to follow them, as long as they’re reasonable. Without a living will, it's up to your doctors, family members, and state law to choose what healthcare you receive.
A living will can also be called a “medical directive” or an “advance healthcare directive.” Despite its name, it shouldn’t be confused with a last will and testament. While a will is used after you die to distribute your property according to your wishes, a living will is used while you’re alive but unable to communicate. With a living will, you prepare for potential incapacity by explaining what kind of healthcare you do or don’t want to receive.
All states have laws regarding when to withhold or withdraw life-sustaining treatment for patients. These guidelines may differ from your personal wishes or beliefs. If you feel strongly about when you do or do not want to receive life-sustaining treatment, consider creating a living will.
2. Medical power of attorney (POA)
A durable medical POA lets you give someone authority to make healthcare decisions for you if you’re unable to express your wishes for yourself. This person may be called your healthcare agent, healthcare surrogate, proxy, representative, or attorney-in-fact.
A durable medical POA can also be called a “healthcare power of attorney” or “durable power of attorney for healthcare.”
3. Advance healthcare directive
Many people choose to pair a living will with a durable medical POA to make sure their future healthcare decisions are handled according to their wishes and by someone they trust. This combination of documents is often called an advance healthcare directive.
First, you use your living will to outline your healthcare preferences. Then, your healthcare agent can use the power you give them in your durable medical POA to make important decisions about anything not covered in your living will (for example, a new surgical procedure).
Your living will’s authority overrides the authority of your medical POA. This means your healthcare agent and doctors must consider the instructions in your living will while making decisions about your healthcare, and reasonably follow those instructions to the best of their ability.
For example, imagine your spouse is your healthcare agent and wants you to have a feeding tube put in while you’re in a coma. However, you expressly stated in your living will that you don’t want to be intubated. As a general rule, doctors will honor what’s in your living will above your spouse’s personal feelings.
4. Psychiatric advance directives
Psychiatric advance directives (PAD), also called “advance directives for mental healthcare,” are becoming more common as society places a greater emphasis on mental wellness. A PAD is a legal document that lets you detail your preferences for future mental health treatment. You can also choose someone to make treatment decisions for you if you’re in a crisis and unable to make them yourself. It’s a good idea to check your state laws to decide if it makes sense to document your preferences specifically for mental healthcare treatment.
Additional healthcare forms
The following documents aren’t advance directives, but they’re important healthcare forms that serve a similar purpose. We go over their similarities and differences below.
Physician’s Orders for Life Sustaining Treatment (POLST)
A POLST is a document you and your doctor fill out together that outlines your wishes for end-of-life care, including CPR and feeding tubes. It’s more detailed than a DNR (do not resuscitate) order.
POLSTs are typically used by people who have a terminal illness or are approaching the end of their life. This is because POLSTs cover specific medical treatments that are relevant to a patient’s existing diagnosis. They’re also used by emergency responders.
Emergency responders are trained to promote health and conserve life. When they’re called to a scene, they’ll usually do everything they can to save your life. But for fragile or terminally ill people, life-saving procedures like CPR may cause additional pain, or delay the inevitable. Having a POLST gives emergency responders clear care instructions, and can allow terminally ill patients to communicate their preference for a natural death.
Since you can’t name a healthcare agent in a POLST, it isn’t a substitute for an advance directive. And healthy people usually don’t need a POLST — an advance directive provides enough instruction. You can visit POLST.org for more information about POLST laws in your state.
Do not resuscitate (DNR) order
A DNR order is a document — signed by a doctor at a patient’s request — that indicates the patient doesn’t want to receive CPR. CPR, or “cardiopulmonary resuscitation,” may involve several potentially life-saving emergency procedures, including:
- Mouth-to-mouth breathing
- Chest compressions
- Administration of controlled electric shocks to the heart (known as “defibrillation”)
- Breathing tube insertion (known as “intubation”)
Like POLSTs, DNRs are often used by patients with serious health conditions who would rather have a natural death than receive CPR.
A DNR has a narrow focus. It only answers the question of whether to administer CPR when a patient’s heartbeat or breathing stops. If you want to provide more instruction to emergency responders, a POLST form may be a better fit.
Advance directives help you prepare for the unexpected
None of us know what the future has in store. That’s why advance directives are powerful and empowering. They help you prepare for difficult situations in advance, so you receive healthcare tailored to your personal, spiritual, and philosophical beliefs.
There are several different ways to create an advance directive. Most states offer free forms that you can download and fill out. You can also use an online site like FreeWill to create your advance healthcare directive (which includes a living will and durable medical POA).
Keep in mind that advance directives can go by several names, including:
- Healthcare directives
- Advance medical directives
- Advance care directives
- Designations of healthcare surrogate
States also have different rules about which types of advance directives they accept. Before creating an advance directive, make sure you understand your state’s rules. You don’t have to hire a lawyer to help you write an advance directive, but you may find it useful to talk to one if you have any questions. And if you have any concerns about how certain medical treatments will affect you, consider speaking with your doctor.
Make your free estate plan today

Make your free advance healthcare directive

Make your free durable power of attorney

Make a stock donation today

Make your free revocable living trust










